What Is A Ppo Health Insurance Plan Preferred Provider Organization

Preferred Provider Organization Ppo Ez Insure A preferred provider organization (ppo) is a health insurance plan for individuals and families. ppos involve networks made up of contracted healthcare providers, including doctors, hospitals, and. A ppo plan is a common type of health insurance that partners with a group of clinics, hospitals and doctors to create a network of preferred providers. with ppo insurance, you’ll pay less out of pocket when you get care within that network. you can still see an out of network provider, but you’ll get the most coverage when you stay within.
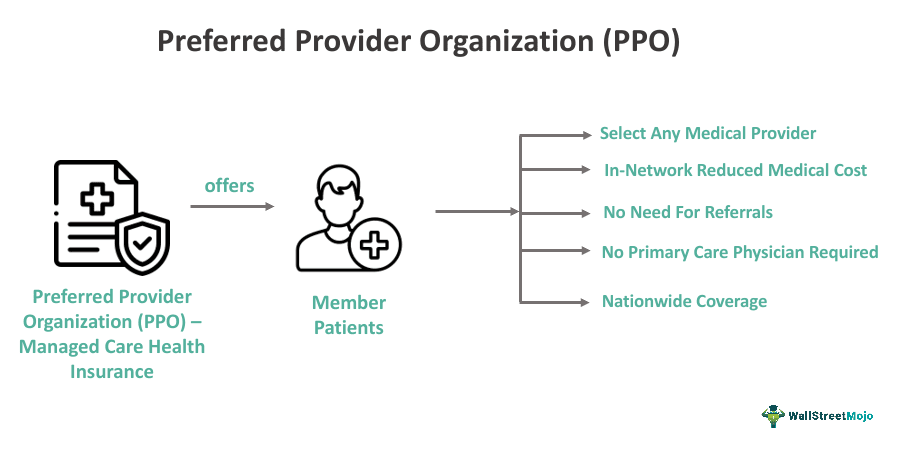
Preferred Provider Organization Ppo What Is It Insurance Plan A ppo is a type of health insurance plan known for its flexibility. insurance companies contract medical care providers and health care facilities to create networks. if you receive care from a. A preferred provider organization, or ppo, is a type of managed health insurance plan. these plans do not require a member to get referrals from a primary care physician in order to see a specialist. and they will cover some of the cost of out of network care, assuming the member has met their out of network deductible (most out of network care. A ppo is a health insurance plan that gives you access to a network of preferred health care providers — physicians, specialists, hospitals, clinics, etc. the insurance company contracts with those doctors and hospitals so that they will charge set prices for certain services. (this system is broadly called managed care.). A preferred provider organization (ppo) is a health plan where an insurance company contracts with hospitals, doctors, and clinics to create a network of participating providers. these providers have agreed to provide medical care to the plan's subscribers at a negotiated rate.
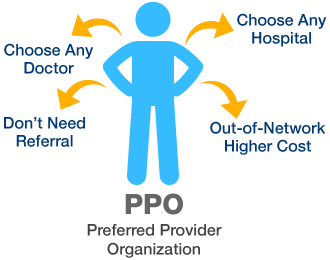
Medicare Basics Definitions Blue Cross Blue Shield Ma A ppo is a health insurance plan that gives you access to a network of preferred health care providers — physicians, specialists, hospitals, clinics, etc. the insurance company contracts with those doctors and hospitals so that they will charge set prices for certain services. (this system is broadly called managed care.). A preferred provider organization (ppo) is a health plan where an insurance company contracts with hospitals, doctors, and clinics to create a network of participating providers. these providers have agreed to provide medical care to the plan's subscribers at a negotiated rate. A preferred provider organization (ppo) plan is a kind of health insurance that gives you flexibility in selecting healthcare providers. you can see any doctor, but you’ll save more by using in network providers. unlike other plans, ppos don’t require referrals to see specialists, allowing easier access to care. Key takeaways: a preferred provider organization (ppo) is one type of network based insurance plan. compared to health maintenance organizations (hmos), ppos offer you more flexibility in choosing the doctors you see, and there’s no need for a referral from a primary care provider. to pay less for care, see doctors, medical professionals, and.
What Is An Epo Hmo And Ppo Florida Health Insurance A preferred provider organization (ppo) plan is a kind of health insurance that gives you flexibility in selecting healthcare providers. you can see any doctor, but you’ll save more by using in network providers. unlike other plans, ppos don’t require referrals to see specialists, allowing easier access to care. Key takeaways: a preferred provider organization (ppo) is one type of network based insurance plan. compared to health maintenance organizations (hmos), ppos offer you more flexibility in choosing the doctors you see, and there’s no need for a referral from a primary care provider. to pay less for care, see doctors, medical professionals, and.

What Is Preferred Provider Organization Ppo Plan

Comments are closed.