Medicare Part D Cms Notification Requirements For Employers Best Nj
Medicare Part D Notification Requirements Best Nj Insurance Part d reporting requirements. this section contains information related to the part d reporting requirements. each part d plan sponsor must have an effective procedure to develop, compile, evaluate, and report information to cms in the time and manner that cms requires. the part d reporting requirements and technical specifications describe. Employers may distribute the medicare part d notice by hand, by mail or by electronic delivery (e.g., email) in a manner that complies with the dol’s electronic disclosure safe harbor. in general, employers must “use measures reasonably calculated to.
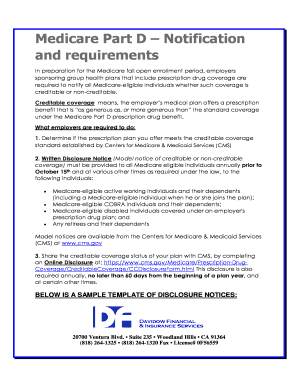
Fillable Online Medicare Part D Notification Fax Email Print Pdffiller Medicare part d, which covers prescription drugs, involves specific reporting responsibilities for employers sponsoring group health plans. it’s crucial for these employers, whether their plans are insured or self insured, to understand and adhere to the requirements set by the centers for medicare and medicaid services (cms) regarding the creditable coverage status of their prescription. Pdf cms model notices. by october 15, prior to commencement of the annual coordinated election period (acep) for part d. employers that provide this disclose to all enrolled employees regardless of medicare status have no obligation to supply a notice when a member turns age 65 during the year (requirement listed directly below). The centers for medicare & medicaid services (cms) provides model notices that employers can use to meet their notification requirements. employers must customize these model notices to include their specific plan sponsor information and ensure each notice accurately reflects the drug coverage status of their plan(s). two separate notices are. Medicare part d notification requirements issued date: 09 20 21 employers sponsoring a group health plan with prescription drug benefits are required to notify their medicare eligible participants and beneficiaries as to whether the drug coverage provided under the plan is “creditable” or “non creditable.” this.

Medicare Part D Notification Requirements Schulman Insurance The centers for medicare & medicaid services (cms) provides model notices that employers can use to meet their notification requirements. employers must customize these model notices to include their specific plan sponsor information and ensure each notice accurately reflects the drug coverage status of their plan(s). two separate notices are. Medicare part d notification requirements issued date: 09 20 21 employers sponsoring a group health plan with prescription drug benefits are required to notify their medicare eligible participants and beneficiaries as to whether the drug coverage provided under the plan is “creditable” or “non creditable.” this. Notice timing. medicare enrollment starts annually on october 15. because the medicare part d notice rules require employers to issue notices before that date, employers must be sure they provide notices by october 14. employers tend to focus on the october medicare part d notices because they relate to a firm, regular deadline. As the enrollment period runs from oct. 15 to dec. 7, the final day to provide this notice is oct. 14. (in years in which oct. 14 falls on a weekend, unlike this year, the due date would be the.
.png?format=1500w)
Medicare Part D Notification Requirements Schulman Insurance Notice timing. medicare enrollment starts annually on october 15. because the medicare part d notice rules require employers to issue notices before that date, employers must be sure they provide notices by october 14. employers tend to focus on the october medicare part d notices because they relate to a firm, regular deadline. As the enrollment period runs from oct. 15 to dec. 7, the final day to provide this notice is oct. 14. (in years in which oct. 14 falls on a weekend, unlike this year, the due date would be the.

Comments are closed.